The combination of central nervous system (CNS) depressants with muscle relaxants is a concern in medical practice, especially considering the potential for enhanced sedative effects. While muscle relaxants and CNS depressants serve different purposes, their interaction can lead to serious side effects and unintended consequences, making it crucial to understand the risks involved.
Understanding the Medications
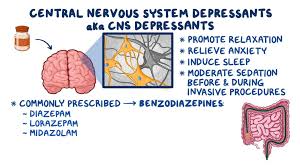
CNS depressants include a wide range of substances, such as benzodiazepines, opioids, alcohol, and barbiturates, all of which work by slowing down brain activity. They are often prescribed for conditions like anxiety, insomnia, and pain management. Muscle relaxants, on the other hand, are typically used to alleviate muscle spasms and pain resulting from injuries or certain medical conditions, such as back pain, fibromyalgia, and multiple sclerosis. These medications, such as carisoprodol, cyclobenzaprine, and methocarbamol, act on the central nervous system to reduce muscle tension.
While each of these classes of drugs can provide relief, their combination can produce a dangerously enhanced sedative effect, leading to adverse outcomes that can put a patient’s health at significant risk.
Sedation and Respiratory Depression
The primary risk when combining CNS depressants and muscle relaxants is excessive sedation. Both CNS depressants and muscle relaxants are designed to calm the nervous system, leading to drowsiness, dizziness, and sedation. However, when used together, these effects can be magnified, leading to profound sedation. This may result in an inability to concentrate, perform normal daily activities, or operate machinery. More critically, it can cause respiratory depression, where breathing becomes slow and shallow or even stops entirely.
Respiratory depression is particularly concerning because it can lead to life-threatening conditions, such as hypoxia (lack of oxygen in the body), brain damage, or even death. This is especially dangerous in individuals who may already have respiratory conditions like chronic obstructive pulmonary disease (COPD), asthma, or sleep apnea.
Impaired Motor Function and Coordination
Muscle relaxants often impair motor coordination by decreasing the tone and tension of muscles, while CNS depressants can affect motor control by inhibiting the brain’s ability to send signals to the muscles. When these two types of drugs are taken together, the effects on motor function can become unpredictable and dangerous.
Patients may experience difficulty with walking, standing, or performing everyday tasks such as driving or cooking. The increased risk of falls, accidents, and injuries can lead to serious physical harm, particularly in older adults who may already have balance issues.
Cognitive Impairment and Memory Loss
Combining CNS depressants and muscle relaxants may also impair cognitive function. Both classes of drugs have the potential to affect memory, attention, and cognitive processing. This can lead to confusion, difficulty concentrating, or forgetfulness, which can have a significant impact on a patient’s ability to function in daily life.
When these drugs are combined, the cognitive effects can be magnified, leading to severe impairment that can interfere with work, social interactions, and other aspects of life. In some cases, this combination can increase the risk of accidents or dangerous decision-making, such as driving under the influence.
Risk of Addiction and Dependence
Another concern when combining CNS depressants and muscle relaxants is the potential for addiction and physical dependence. Many CNS depressants, such as benzodiazepines and opioids, carry a risk of dependence when used long-term or inappropriately. When taken with muscle relaxants, the sedative effects can make these medications more desirable, increasing the risk of misuse.
Patients may develop a tolerance to both CNS depressants and muscle relaxants over time, meaning that higher doses will be required to achieve the same effect. This increases the likelihood of substance abuse and may lead to serious withdrawal symptoms if the drugs are discontinued suddenly.
The psychological aspect of dependence can also be a concern, as patients may begin to rely on the combined effects of these medications for emotional or physical comfort, which can perpetuate the cycle of use and misuse.
Interaction with Other Medications
Both CNS depressants and muscle relaxants can interact with other medications, complicating treatment and increasing the risk of adverse effects. For instance, certain antidepressants, antihistamines, or antipsychotic medications can also depress the CNS. When these drugs are combined with muscle relaxants, the risk of sedation and cognitive impairment can increase significantly.
Patients who are taking multiple medications may find it challenging to manage the interactions between them, and health providers may not always be aware of every medication a patient is using. This underscores the importance of clear communication between patients and healthcare providers about all medications being taken, including over-the-counter drugs, supplements, and alcohol.
Increased Risk in Vulnerable Populations
Certain populations are particularly vulnerable to the risks of combining CNS depressants with muscle relaxants. Older adults, in particular, are at greater risk due to age-related changes in the metabolism of medications. As people age, their bodies process medications more slowly, which can lead to higher concentrations of the drugs in the bloodstream and increased side effects.
Furthermore, older adults are more likely to have other chronic conditions, such as hypertension, diabetes, and arthritis, which may complicate the use of multiple medications. The combination of CNS depressants and muscle relaxants can exacerbate conditions like dementia, cognitive decline, and balance problems, further increasing the risk of harm.
Pregnant and breastfeeding women are also advised to avoid this combination, as both CNS depressants and muscle relaxants can cross the placenta and affect the developing fetus or newborn. These medications may cause developmental delays, low birth weight, or other complications.
Conclusion
The combination of CNS depressants with muscle relaxants can provide short-term relief for specific conditions, but it comes with significant risks. The synergistic sedative effects of these drugs can impair motor function, cognitive abilities, and respiratory function, leading to dangerous outcomes such as falls, accidents, and respiratory arrest. Additionally, the combination can increase the potential for addiction, dependence, and harmful drug interactions.
Patients who are prescribed both CNS depressants and muscle relaxants should work closely with their healthcare provider to ensure safe and appropriate use. This may include adjusting dosages, considering alternative medications, or monitoring for signs of adverse effects. Health providers must also educate patients about the potential risks and provide strategies to minimize harm, such as avoiding alcohol or other CNS depressants and not operating machinery while on these medications.
Ultimately, while CNS depressants and muscle relaxants can be effective in managing specific health issues, their combination requires careful consideration to prevent serious complications.